You are here
Tardive Dyskinesia
What is tardive dyskinesia?
To learn more about Living With TD, click here.
Tardive dyskinesia is a neurological disorder caused by the long-term use of neuroleptic drugs, or anti-psychotic medications. Neuroleptic drugs are generally prescribed for psychiatric disorders, as well as for some gastrointestinal and neurological disorders. Neuroleptic drugs work by blocking dopamine receptors in the brain. Dopamine is a neurotransmitter that helps control the brain’s reward and pleasure centers but also plays a major role in motor functioning. As a result, neuroleptic drugs can cause disorders affecting the motor system.
- Infographic: Tardive Dyskinesia: A Serious Side Effect
- Infographic: 5 Steps For Taking On Tardive Dyskinesia
- Patrick's Story: I have Tardive Dyskinesia, but I am one of the lucky ones
How common is tardive dyskinesia?
Tardive dyskinesia is estimated to affect at least 500,000 people in the U.S.[1]
Those who have been treated for schizophrenia, schizoaffective disorder, and/or bipolar disorder are particularly at risk.
The older a person is, the more likely they are to develop persistent and irreversible tardive dyskinesia.
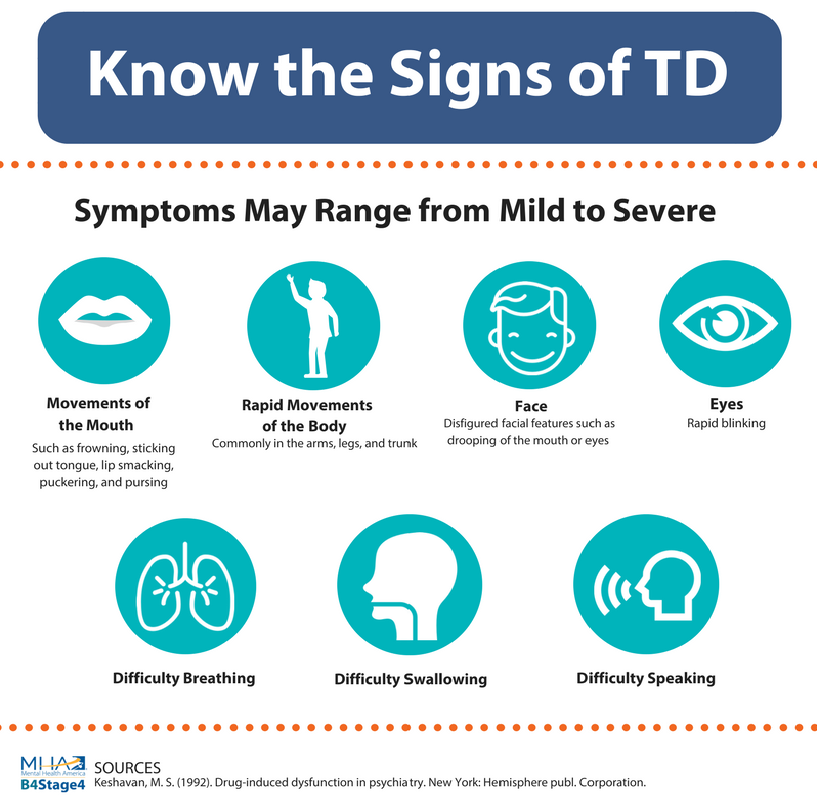
Tardive dyskinesia is characterized by repetitive and involuntary movements.
Features of the disorder may include:
- Frowning
- Tongue sticking out
- Lip smacking
- Puckering and pursing of the lips
- Rapid eye blinking
- Rapid movements of the arms, legs, and trunk may also occur.
Approximately 60 to 70 percent of the cases are mild, with about 3 percent being extremely severe.
Severe cases may involve problems such as difficulty swallowing, speech interference, disfigured facial features, and breathing trouble.
Download this questionnaire to see if you, or someone you love may be experiencing signs of tardive dyskinesia.
Tardive dyskinesia and Parkinson's disease: What's the difference?
Tardive dyskinesia is not to be mistaken with Parkinson’s disease. Tardive dyskinesia and Parkinson’s disease are both classified as movement disorders and are linked to dopamine.
While they both can result as a side effect of medication, the similarities stop there.
The symptoms of tardive dyskinesia are opposite of those associated with Parkinson’s. People with Parkinson’s have difficulty moving whereas tardive dyskinesia patients have difficulty not moving.
Additionally, the movements associated with tardive dyskinesia are more fluid and less jerky than spasms and stiffness experienced by those with Parkinson’s.
What can cause Tardive dyskinesia? [2]
Drugs that most commonly cause this disorder are older neuroleptics, including:
- Chlorpromazine (Thorazine or Largactil)
- Fluphenazine (Prolixin, Modecate, or Moditen)
- Haloperidol (Haldol)
- Perphenazine (Trilafon, Etrafon, Triavil, or Triptafen)
- Prochlorperazine (Compro, Darbazine, or Neo Darbazine)
- Thioridazine (Mellaril)
- Trifluoperazine (Stelazine or Stelbid)
These are not the the only medications that can cause TD. Newer drugs that may cause tardive dyskinesia (although are less likely to cause it) include:
Antidepressants
- Amitriptyline (Elavil)
- Fluoxetine (Prozac)
- Phenelzine (Nardil)
- Sertraline (Zoloft)
- Trazodone (Desyrel or Oleptro)
Other drugs
- Metoclopramide (Reglan or Metozolv ODT) which treats gastroparesis
- Levodopa (Larodopa or Dopar) which treats Parkinsons
- Phenobarbital (Luminal or Solfoton) which treats seizures
- Phenytoin (Dilantin or Phenytek) which treats seizures
How is it treated?
There is no standard treatment for tardive dyskinesia. Most interventions focus on adjusting the medication thought to be causing tardive dyskinesia. In many cases neuroleptic medications will be adjusted to use the lowest possible dose, or discontinued if at all possible. Stopping the medication is a gradual process, lowering the doses 10 to 25 percent every one to three months. Replacing the neuroleptic drug with other medications may help some patients. Other drugs such as tranquilizers like benzodiazepines and medicines that mimic the effect of dopamine, may also be beneficial. Symptoms of tardive dyskinesia may remain even after the medication is stopped. However, with careful management, some symptoms may improve or disappear with time.
Tardive dyskinesia symptoms may take time to develop. On some occasions symptoms do not arise until after neuroleptic drug use has been stopped. For this reason, tardive dyskinesia may be hard to diagnose. If you think you have tardive dyskinesia seek medical attention through a neurologist. For a diagnosis, doctors should evaluate the length of neuroleptic drug exposure. Exposure does not need to be consistent but should continue for three or more months of use. They should also rule out other conditions that cause movements such as Parkinson’s or Cerebral Palsy and recognize symptoms in two or more body areas. [3]
New treatments for tardive dyskinesia have been developed and work by reversibly limiting the amount of excess dopamine. While these treatments have not been around long, they have shown great promise in clinical trials. If taking psychiatric medications, these new drug treatments for TD are meant to be taken in addition to existing medications.
Other Resources
Tardive Dyskinesia/ Tardive Dystonia National Assoc.
P.O. Box 45732
Seattle, WA 98145-0732
Phone Number: (206) 522-3166
National Institute of Mental Health
Phone Number: 301-443-4513
Toll Free Number: 1-866-615-6464
Fax Number: 301-443-4279
Email Address: nimhinfo@nih.gov
Website URL: www.nimh.nih.gov
National Org. for Rare Disorders (NORD)
P.O. Box 8923
New Fairfield, CT 06812-8923
Phone Number: (203) 746-6518
Toll-Free Number: (800) 999-6673
Website URL: www.rarediseases.org
[1]Cloud LJ, Zutshi D, Factor SA. Tardive dyskinesia: therapeutic options for an increasingly common disorder. Neurotherapeutics. 2014;11(1):166-176.
[2] Tardive Dyskinesia. Retrieved from https://medlineplus.gov/ency/article/000685.htm
[3] (2013). Treating and Managing Tardive Symptoms Retrieved July 18, 2017, from https://www.aan.com/Guidelines/Home/GetGuidelineContent/614







this page